Cognitive Disorders
Cognition:
The process of obtaining, organizing, and using intellectual knowledge and understanding the connection between cause and effect, between action and its consequences.
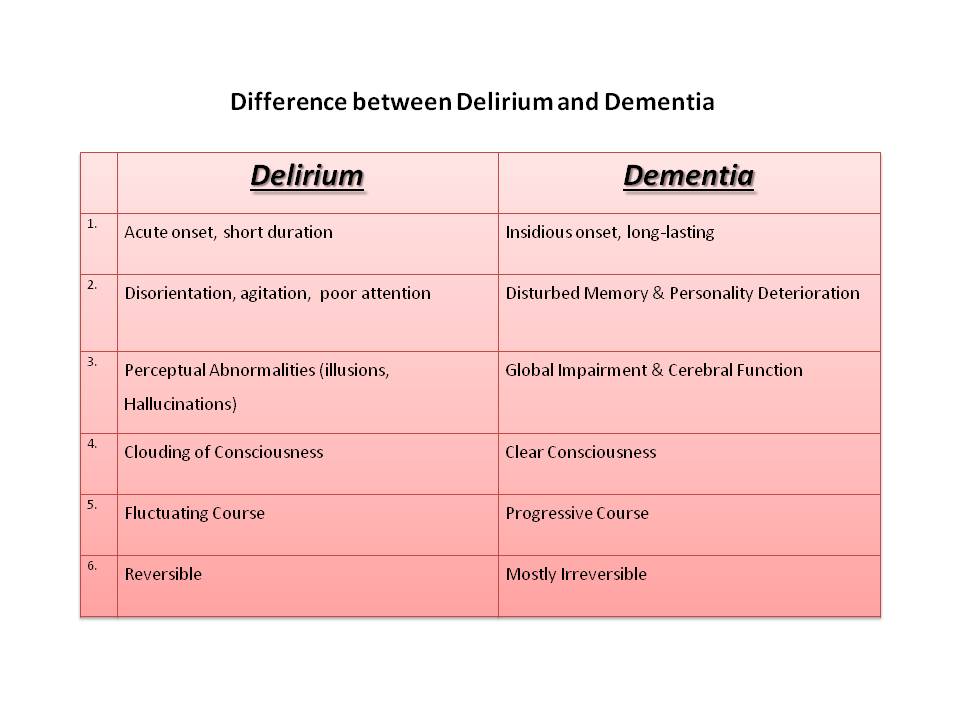
Delirium, Dementia, and Amnestic disorders are the groups of conditions where the core symptom is cognitive dysfunction.
Delirium:
Delirium is a syndrome, not a disease, caused by the sudden change in brain function due to an underlying cause leading to confusion, emotional disturbances, altered sleep and appetite pattern.
It is a sudden onset, last less than a few days, always due to an underlying medical or neurological cause.
It is divided into four categories based on causes
- Delirium due to the general medical condition
- Delirium due to substance use
- Delirium due to multiple causes
- Delirium not otherwise specified
Core symptoms of Delirium:
- Impairment of consciousness: reduced level of consciousness, reduced attention, inability to focus or sustain or shift attention
- Cognitive dysfunction: disorientation with respect to time, place and person, impaired memory, impaired judgment
- Impaired thinking: tangentially and incoherence speech
- Perceptual disturbances: illusions and hallucinations- visual, auditory, tactile are common
- Sleep disturbances: altered sleep-wake cycle, fragmented sleep, and nighttime awakening
- Mood swings: irritability, euphoria- dysphoria
- Psychomotor activity: increased and decreased within a day
- Autonomic hyperactivity: sweating, increased blood pressure
Risk factors for Delirium
- Elderly
- Brain damage
- Underlying medical or surgical condition or neurological condition
- Sleep deprivation
- Prolonged surgery, immobility
- Electrolyte imbalance
- Vitamin deficiencies: B1, B6, B2. B12, folic acid
Aetiology of Delirium:
- Brain trauma,
- Brain tumour,
- Cerebro-vascular disease – infarction, haemorrhage
- cerebral infections- meningitis, encephalitis
- Substance abuse and withdrawal
- Certain drugs: anticholinergics, steroids
- Endocrine dysfunction- hypo/hyperfunction of pituitary, pancreas, thyroid, parathyroid, adrenal glands
- Dysfunction of liver, kidney, lungs, heart
- Systemic infections: Fever and sepsis
Management of Delirium:
The syndrome of delirium is considered secondary to an underlying medical/neurological/surgical condition which has to be thoroughly investigated and treated
Example: liver abscess—fever, electrolyte imbalance, elevated liver enzymes- treat it with appropriate antibiotics
Symptomatic treatment includes:
- control of agitation with Lorazepam or Haloperidol
- Maintaining fluid and electrolyte balance
- Adequate nourishment
- Rest, reassurance, support
Prognosis:
Delirium is always sudden and generally last less than a week
Once control of causative factors is achieved (ex: meningitis), improvement symptoms recede within 3-7 days
Older the patient, multiple causes, untreatable medical/surgical conditions (ex: liver cancer) carries increased mortality in the subsequent year.
DEMENTIA
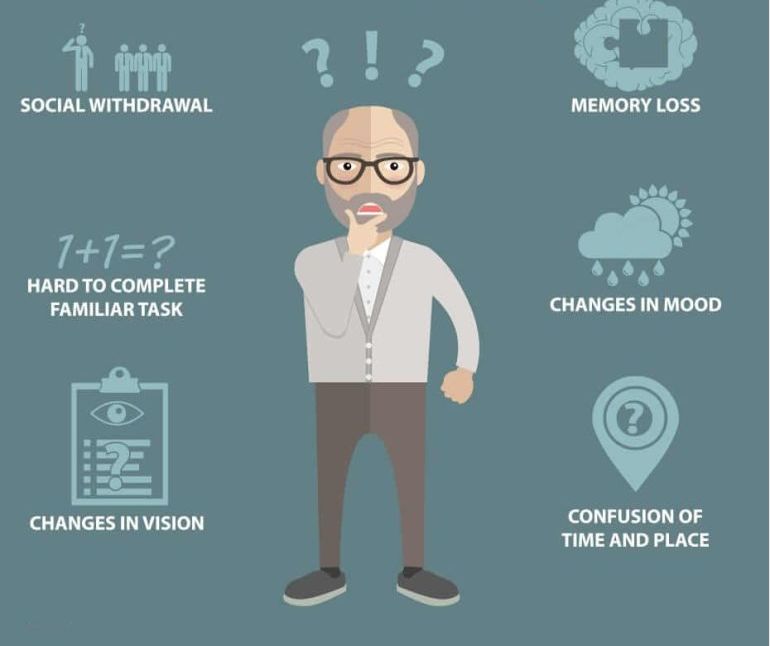
Dementia is a syndrome in which there is deterioration in memory, thinking, behaviour and the ability to perform everyday activities. It is gradual in onset, more prevalent as age advances; usually, the conscious level is maintained.
For example, at 80 years, prevalence is about 2-3%, beyond 85 years, it’s about 8%
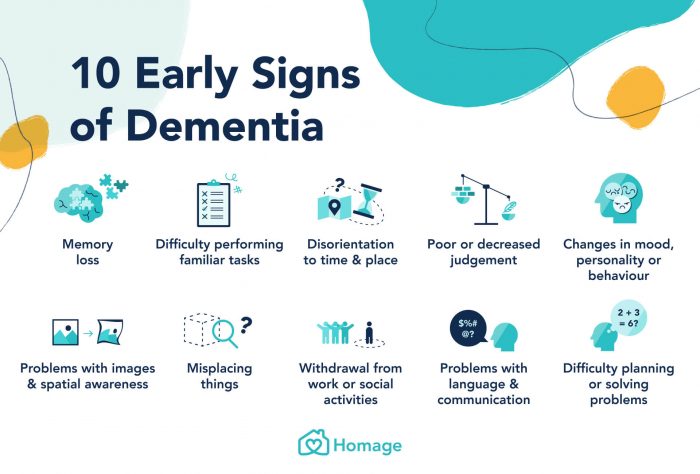
The cognitive disturbances include
- Impairment in memory
- Language disturbances- aphasia
- Inability to carry out the routine task- apraxia
- Failure to recognize or identify objects-agnosia
- Disturbances in executive functions such as planning, organizing, sequencing, abstracting
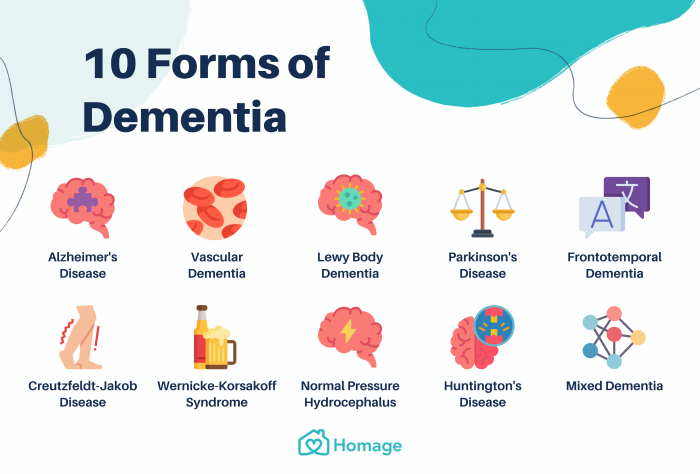
Types of Dementia:
- Dementia of Alzheimer’s type
- Vascular Dementia
- Picks disease
- Lewy body disease
- Huntington’s disease
- Parkinson’s disease
- HIV related to Dementia
- Head trauma-related Dementia
Alzheimer’s Dementia
The most common form of Dementia- up to 60%
The cause is unknown- genetic factors- abnormal genes in chromosomes- 21, 14, 19
The pathology is a loss of neurons, loss of synapses, loss of neurotransmitters, its receptors
There is a loss of water within the cells, and there are areas of empty space filled with inactive fibres- called neurofibrillary tangles and senile plaques.
There is a progressive memory disturbance
Mild Dementia or early stage
Persons during the early phase of Dementia maybe
- Forgetting recent events, telephone numbers, personal belongings, name of common objects of daily use, name of the person whom they have met recently
- Fail to identify common colours, address,
- Clumsy while driving, climbing stairs
- Forget to close the door, switch off the fan, gas knob.
- May forget to add the required ingredients while cooking
- They may substitute explanation over words ex: four-legged object for writing instead of “TABLE.”
Moderate Dementia:
- Unable to do a routine task like driving, cooking
- Couldn’t identify familiar persons, common objects,
- Unable to work or continue in a job
- Difficulty in daily activities like bathing, dressing, fetching things from a nearby shop
- Does not aware of the day, date, month
- Easy irritability, emotional lability, especially when mocked about the memory loss
- Depression, paranoid towards the caregivers, neighbours
Severe Dementia
- The above symptoms become exaggerated, and the person may not be able to identify their own family members, often who they are?
- Associated with motor in-coordination- stumble while walking, climbing stairs, frequent fractures
- Self-care and hygiene becomes poor
- Needs to be fed, to be dressed, yet they won’t allow for it
- Often aggressive, agitated and pounce back towards the caregivers
- May try to run away and may not find way back home
Terminal stage:
- They are bedridden, develop bed sores or Infections
- Aspiration is a common cause of death
Prognosis: the average survival expectation once diagnosed as Alzheimer’s Dementia is approximately 8 years
Vascular Dementia:
The second most common form of Dementia
It is due to multiple infarcts in the brain that occurs over years
These patients have uncontrolled hypertension, diabetes, dislipidemia
History of smoking, alcohol dependence, obesity is common
CT or MRI brain shows multiple parenchymal lesions throughout the brain
Memory disturbances that occur are sudden and stepladder fashion than progressive
Lewy body dementia.
This is one of the common types of progressive Dementia, with predominant perceptual symptoms like visual hallucinations, gait disturbances apart from the decline in memory and executive dysfunction. The brain cells are replaced by clumps of protein seen in the microscope as “Lewy body.”
Frontotemporal dementia.
Here the degeneration of nerve cells is more in the frontal and temporal lobes of the brain. Hence there is personality deterioration, behavioural abnormalities, judgement and language difficulties during the earlier phase
Pick’s Disease
- Asymmetric atrophy of the frontal and temporal lobes
- Personality change is common
Complications in Dementia:
Dementia is a neurological disorder with progressive loss of brain cells; thus, the function of these cells or neuronal areas affected gradually; psychiatric manifestations are common along with memory decline.
Common symptoms are
- Depression
- Paranoid symptoms – Delusions and hallucinations
- Behavioural disturbances called “BPSD – Behavioural and psychiatric symptoms of Dementia” where the person show changes in personality, thinking, behaviours, social functioning, and self-care
- Wandering tendency
- Hypersexual paraphilia could occur
- Aggression
- Erratic sleep and appetite pattern
- Non-compliance with caregivers leading to marked caregiver distress and abuse/neglect
Diagnosis:
Any elderly patient who is found to have a history suggestive of memory loss, change in mood or personality should be appropriately investigated for signs of early Dementia.
Mini-mental status examination (MMSE) is a 30 item questionnaire that helps to identify suspected cognitive dysfunctions
Investigations aimed to identify the possible reversible causes of Dementia
- B12 levels
- Thyroid function, liver function, renal function tests
- Check Blood pressure, blood sugar, blood cholesterol levels
- CT or MRI brain helps to identify the extent and severity of Dementia
Pseudodementia vs Dementia.
- Pseudodementia is a symptom commonly seen in depression and during stress.
- Here the patient is excessively preoccupied with memory loss and constantly attempts to check what they have forgotten or remembered.
- Usually, they complain of loss of memory for names of people, misplacing household things.
- Upon testing for the memory, they usually answer “I don’t Know” and give a detailed account of what they have forgotten these days. Simultaneously, a true patient with Dementia found to give wrong answers or may turn irritable during testing.
- There is a fear that they have lost their mental function and insists on a thorough checkup, brain scans etc.,
- The condition is due to indecisiveness and inability to concentrate on routine activities seen in depression
Management of Dementia
Reversible Dementia vs irreversible Dementia
Up to 10-15% of Dementia is reversible when treatment is initiated before permanent brain damage
Causes: hypothyroidism, normal pressure hydrocephalus, brain tumour, B12 deficiency
Drug Treatment
No Specific Drugs that will cure the condition or reverse into the original state, effective control of Hypertension and Diabetes will reduce further progression.
Certain recently introduced drugs show improvement in cognitive functions and delay further progression.
- Donepezil (5-10mg),
- Rivastigimine( 1.5-6mg),
- Galantamine(4-12mg),
- Memantine(15-10mg).
Antioxidants such as vitamins A, C, E, B12 can reduce progression.
Psychosocial Management
- Behavioural Methods- active orientation of day, time
- Activity Engagement- self-care, daily teaching activities, personal hygiene
- Physical Exercise
- Problem-Oriented Approach
- Reality Orientation
- coordination of Psychiatric, neurological, medical services
- Nursing care
- Caregivers Support and education
Nursing Care for Dementia
- Assess Patient’s Level of Functioning
- Nurse the Patient in Familiar Surrounding
- Due to Disorientation patient may be wandering -Advice to tie ID-Card
- Simple explanation & face to face Instruction
- Limit noise, visitors
- Allow stimuli- appropriate sunlight
- Maintain hydration
- Reassurance
- Educating the Caregiver
Prevention:
It is said the process of neuronal loss starts as early as 20 years of age, and it’s evident only after 65 years of age hence
Youngsters should
- Maintain weight
- Physical exercises- sports, yoga, meditation
- Avoid smoking, alcohol
- A balanced diet with plenty of fresh fruits and vegetables
Adults and elderly
- Should check and seek appropriate management for hypertension, diabetes, dislipidemia
- Actively engage in learning new skills
- Regular physical exercise- yoga, brisk walk
Story of a Math’s Teacher
Mr Ram was born in 1941 in a town near Trichy; his father was a farmer, so his mother had three younger brothers and 2 younger sisters. He was the first child who had studied in Tamil medium school up to 5th grade and was sent to study in Trichy in English medium, and he was above average in studies, secured 79% in X and 82% in XII standard. He was interested in math’s and joined BSc mathematics in Trichy, secured first class in this and continued to study MSc maths and B’ed. He soon got a job and started his carrier as a math’s teacher; his passion for mathematics continued, he was a strict teacher, and he used to solve any sum from 1st grade to 12th-grade syllabus, and students would keen on learning from him, even after the school timings.
His goal was to make every student pass in his subjects and take special classes and free tuitions for students who needed it. But was short-tempered and would trash naughty students. He had a good reputation from his fellow teachers; some were even envious of his school popularity. He started smoking cigarettes at the age of 22 and now would smoke up to 10 per day, though he wouldn’t smoke in students’ presence. After he settled his brothers and sisters in the right place, he got married at 35. One of his brothers was a BE graduate and got a job in an MNC company in Chennai and within a year flew to the US, and the other two ended up doing father work.
He had two daughters, and his wife felt he loses temper soon and consulted a physician, who found his blood pressure persistently high, and advised medications, exercise and quitting smoking. Due to his hectic work- school, evening tuitions, he did not find time to go for a morning walk and unable to quit smoking. He continued taking the prescribed medications. His parents passed away; consequently, he distributed his father’s land to his younger brothers and sisters, who were not educated and dependent on agriculture within a couple of years. Following his parent’s death, all his younger siblings moved to a nuclear family.
He moved to Trichy, rented a house, his daughters were studying in private schools, continued to work in the same school, took tuitions for the needed and thus his day starts with teaching maths from 9 AM to 8 PM. Even during Sundays, he would take special tuitions for students from other schools as well. He continued to smoke now up to 15 per day. Though he maintained weight, his blood pressure remained high. Towards his retirement, he got both of his daughters married, one in Chennai and another in Pudukottai.
He lived with this wife, continued to take tuitions. He continued to smoke, and at 62 years of age, he developed chest pain, and his physician diagnosed him with angina, prescribed medications and advised him to stop smoking. Mr Ram, though he took medications, but couldn’t stop smoking, yet reduced by half. Due to his health conditions, his wife and daughters did not allow him to take tuitions, took him to Chennai, found an apartment for the couple.
Mr Ram felt lonely in the new city, with heavy traffic and no other work, he spent time watching TV and reading newspapers. No friends here and felt depressed. Gradually he was found dull, less interactive, irritable, eating less and sleepless nights. A year passed by he was taken to a psychiatrist in Chennai, who diagnosed him with clinical depression prescribed antidepressants and sedatives. His sleep improved, irritability reduced, and he was interactive, yet he was not fully recovered. He longed for his passion for teaching maths to students. Years passed by, at 69 years of age, his wife found him dull more, lazy, retarded and irritable and assisted him, did not allow him to go out.
She found him misplacing his personal belongings like a watch, spectacles and searching, even getting suspicions that someone is stealing these belongings. Scolded his wife for misplacing his things. He was moody would play well with his grandchildren or often locks himself in the bedroom. He had a memory disturbance that would misidentify his grandchildren of both of his daughters.
Once they had been to “Tirupathi”, and in the crowd, he was lost, after nearly five hours of announcement and search he was found in anther end, he could not tell his address or phone number. Upon returning, his wife took him to their psychiatrist, who suspected early Dementia and sought a neurologist opinion. His scan report showed diffuse cerebral atrophy; he was prescribed medications. Days passed by, he was found deteriorating in his memory and could not tell names of his daughters, sons-in-law, his address, and unable to tell what he needed.
His wife has to feed him, bathe him by force. Physicians psycho educated it was Alzheimer’s Dementia, and it has a deteriorating course, yet the medications would only reduce the progress a bit. Within 3 years of diagnosis of Dementia, he was so impaired needed assistance in daily activities like bathing, dressing, feeding.
He has lost all his mathematical abilities, unable to do simple calculations, even addition or subtraction. His wife was depressed, and the psychiatrist has to prescribe antidepressants for her. At 72 yrs, they shifted back to his hometown, where his father lived. He couldn’t identify his brothers or sisters, and none helped, took a rented house, and his wife alone cared. Many of his old students and colleagues came to visit him, none he could recognize; once he was invited to the school function where he worked, he just sat on the stage ideally couldn’t deliver a speech.
Once, he tripped while getting down from his house and sustained a fracture of the hip. Orthopaedic suggested hip replacement due to severe osteoporosis, which costs 2 lakhs. He was surviving with a pension of Rs 6000 a month, which she couldn’t afford. None of his brothers helped. He was confiding to bed, and his wife would nurse him, often irritable, spit food on her, cursing her as a devil. He would soil his clothes often, soon developed bedsores, lung infections and diarrhoea.
At his 73 rd year, he once aspirated in his sleep and had his last breath.
Moral from the story- What went wrong? How could this have prevented?
Diagnosis: Dementia
Continued smoking, poor control of hypertension. He was forced to quit his passion, left alone in a crowded city
Neuropsychiatry of Head injury
Head injury is one of the commonest causes of death in road traffic accidents; even if a patient survives, there are ongoing difficulties throughout the person’s life.
It is estimated that nearly 1.5 to 2 million persons are injured, and 1 million succumb to death every year in India.
Road traffic injuries are the leading cause (60%) of Head injury, followed by falls (20%-25%) and violence (10%).
Alcohol involvement is known to be present among 15%-20% of Head injury.
Head injury considered significant when any one or more of the following features are present
- Loss of consciousness (LOC): the duration of LOC is directly proportional to the extent of neuronal damage.
- ENT bleed: bleeding from ears, nose, or throat will denote there is intracranial bleed
- Projectile vomiting
- Seizures following injury
A person recovering from a head injury are more prone to develop
- Depressive disorders
- Anxiety disorders- PTSD
- Psychosis – delusions or hallucinations
- Continue substance dependence
- Cognitive impairment of various degrees depending upon the extent of neuronal damage
- Personality change
Personality change following Head injury
- Childish- in speech and actions
- Talkative
- Self-centred
- Insensitive
- Euphoric-happy and doesn’t worry about future
- Poor judgment
- Helpless-others need to persuade him in his carrier
- Lack of Insight into such behavioural/cognitive problems
Story of a Post-Head Injury Sequelae
Mr K, 42 yr old, working in Govt sector, married with two kids, brought by his spouse with 2 months duration of being restless, not sleeping, continuous talk, easy irritability, abusive, suspicious towards wife and siblings, eats more, frequent alcohol abuse, increased sexual desire, lacks social concerns, spends lavishly, lost all his bank savings and is on medical leave last 4 months.
He was a regular consumer of alcohol over the last 10 years, more in the previous 2 yrs with almost every day while returning home.
About 4 months ago, while on his way back home in a drunken state, he collided over a lamppost, sustained a significant blow to his head, fell unconscious, and regained only on the 13th day in hospital ICU. His medical records showed significant brain injury (bilateral frontal lobe damage) and were operated on to arrest the bleeding. He recovered and was discharged after 5 weeks in the hospital, and his spouse had to spend 2.5 lakhs as medical expenses alone.
The patient was admitted to our hospital. Psychological workup and cognitive assessment showed memory and functional dysfunction secondary to the irreversible Brain damage
Diagnosed as Post Head injury Personality change
The patient was hospitalized for 2 weeks, with little or no improvement. He could sleep well with medications, agitation, craving for alcohol, irritability and cognitive dysfunction.
Conclusion: a Person who recovered from significant Brain damage gradually develop changes in their personality- thoughts, mood and behaviour that remain resistant to treatment.
Thus don’t Drink and Drive; wear a helmet