Total Visitors
Athma Mind Care Hospital supports individuals dealing with persistent physical symptoms linked to emotional stress. As one of the trusted centres for somatoform disorder treatment in Chennai, our goal is to help patients understand their symptoms, reduce discomfort, and regain daily functioning.
We follow structured somatoform disorder therapy designed to lower anxiety, improve clarity, and build long-term stability.
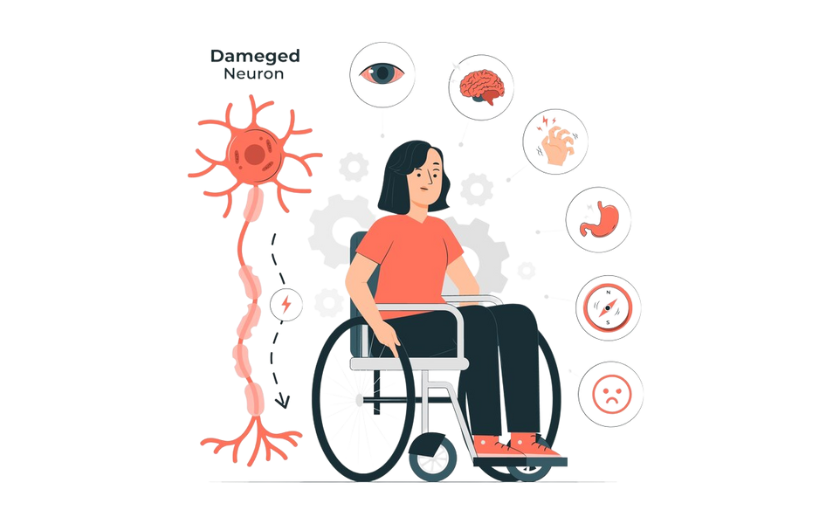
Somatoform disorder, also called somatic symptom disorder, involves physical symptoms that continue even when medical tests show no specific cause.
At our centre, offering somantic disorder treatment in Chennai, specialists study the link between stress, emotions, and physical sensations.
This helps us design a treatment plan that focuses on both physical relief and emotional balance.
Seek help at our hospital if you notice
Our team provides early somantic symptom disorder diagnosis and treatment to prevent symptoms from turning chronic and to support faster recovery.
A psychiatrist guides patients through understanding their symptoms and the emotional factors behind them. They provide counselling, teach coping methods, and work with families to improve support at home.
Our team helps you to lower your distress, improve resilience, and helps patients handle symptoms more effectively.
Our treatment approach includes:
This structured care model supports individuals seeking reliable somatoform disorder treatment in Chennai.
Our specialist provides therapy, which plays a major role in recovery.
Our programs include:
Consistent somatoform disorder therapy helps patients gain control over symptoms and improve daily functioning.
Rehabilitation focuses on long-term stability and independence. Patients receive:
These services strengthen coping skills and improve quality of life over time.
Early somantic symptom disorder diagnosis and treatment help avoid unnecessary medical tests and reduce the cycle of worry and discomfort. It provides patients with a clear understanding of their condition and speeds recovery.
Misunderstanding often affects individuals dealing with somatoform symptoms.
At Athma Mind Care Hospital, we aim to create awareness and encourage families to approach these symptoms with empathy.
Supportive environments help patients recover faster and with greater confidence.
Athma Mind Care Hospital is committed to helping patients build strength, clarity, and stability. We focus on emotional health, symptom control, and continuous guidance, with compassionate care and structured treatment, we help individuals move toward a balanced and healthier life.
Connect with our expert doctors and therapists today and take the first step toward a calmer, healthier life.
Ready to take the next step in your mental health journey? Scheduling an appointment with us is easy!
If you are in crisis or need immediate support, our 24/7 emergency counseling service is here for you. Our trained professionals are available around the clock to provide assistance, guidance, and support during difficult times.